Middlefield (860) 349-8500
Wallingford (203) 294-4977
Middlefield (860) 349-8500
Wallingford (203) 294-4977
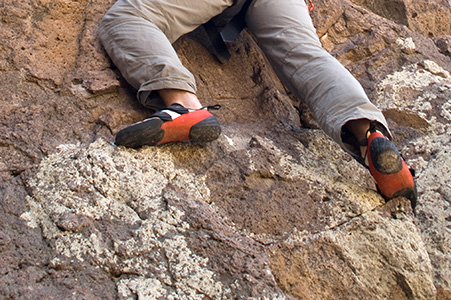
Foot injuries from rock climbing are more common than many people think, especially during falls or from wearing tight climbing shoes. Falls can lead to bruises, sprains, or broken bones in the heel or ankle, which may require surgery to heal properly. However, repeated impact and pressure from tight shoes can also cause long-term problems. These include pain in the toes, thickened skin, and blood under the toenails. Many climbers wear shoes that are too small in order to get a better grip, but this can change how the foot moves and put too much pressure on certain areas. Over time, this can lead to chronic foot pain and deformities that may limit movement or cause discomfort even when not climbing. Changes in toe shape, such as bunions, or stiffness in the big toe joint may also develop. A podiatrist can diagnose climbing-related foot and ankle injuries, help manage pain, and recommend the best medical treatment, which may include surgery if needed. If you have injured your foot while rock climbing, whether indoors or outside, it is suggested that you make an appointment with a podiatrist for treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Swollen ankles are often caused by a buildup of fluid in the soft tissues, known as edema. This can develop for many reasons, including standing or sitting in one position for too long, consuming high amounts of salt, being overweight, pregnancy, or taking certain medications. Swollen ankles may also result from an ankle sprain, infection, insect bite, or more serious conditions involving the heart, kidneys, or liver. Symptoms can include puffiness around the ankles and feet, shiny or stretched skin, skin discoloration, and discomfort or stiffness. In some cases, pressing the skin may leave a dent. A podiatrist can perform a detailed exam to determine whether the swelling is linked to an injury, circulation problem, or another medical condition. Depending on the cause, treatment may involve reducing inflammation, draining excess fluid, prescribing medication, or correcting biomechanical issues with the foot or ankle. In severe or persistent cases, surgery may be recommended to resolve structural or vascular concerns. If you have swollen ankles, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and appropriate treatment.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Dr. Gordon Fosdick of Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
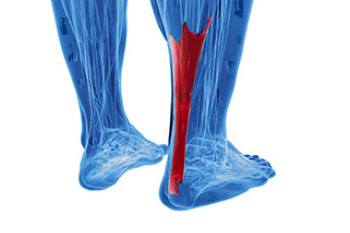
An Achilles tendon tear is a painful injury that often occurs during activities that involve sudden starts, stops, or pivots, especially in sports or while running. The Achilles tendon, which connects the calf muscles to the heel bone, is essential for walking, running, and rising onto the toes. A torn Achilles tendon may happen suddenly, often with a popping sound, followed by sharp pain at the back of the ankle. Patients may find it difficult to push off the foot or stand on their toes. In many cases, the foot may exhibit abnormal movement, including excessive pronation or supination, which can place strain on the tendon. A podiatrist can examine your ankle and foot alignment, assess range of motion, and determine the extent of the tear using diagnostic tests. If the tendon is completely torn, surgery may be required to restore function. A podiatrist can also help guide you through non-surgical recovery methods, including immobilization, and provide support for proper foot biomechanics. If you have injured your Achilles tendon, it is suggested that you make an immediate appointment with a podiatrist for an exam, diagnosis, and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Gordon Fosdick of Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.