Middlefield (860) 349-8500
Wallingford (203) 294-4977
Middlefield (860) 349-8500
Wallingford (203) 294-4977

Peripheral neuropathy is a nerve disorder that can affect the feet. It typically causes the inability to feel sensations in the feet, and is prevalent among diabetic patients. Elevated glucose levels can cause neuropathy in the feet, and can be dangerous among diabetics. Neuropathy can affect many types of nerves. The most common are motor, sensory, and autonomic nerves. Motor nerves include those that allow us to walk, talk, and grasp objects. The pain that is felt from a cut is classified as a sensory nerve, and breathing, digestion, and heart functions are in the autonomic nerve category. Muscle weakness is associated with neuropathy, and can be caused by physical injury, arthritis, and diabetes. If you have a lack of feeling in your feet, it is strongly suggested that you are under the care of a podiatrist who can treat and help you to manage neuropathy.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Type 2 diabetes is a serious health condition. It can affect the feet so it is important to check the feet daily for any existing cuts, bruises, or scrapes in order to prevent foot ulcers from developing. Neuropathy can occur with diabetes and it produces a numbing or tingling sensation. This can make it difficult to feel anything on the feet. The diabetic's ability to heal can be diminished and cuts and scrapes can easily become infected. This condition may be controlled by monitoring the blood glucose levels and this can be helped by eating foods that have little or no sugar. It is beneficial to practice proper foot care which includes washing and drying the feet daily and wearing shoes that fit correctly. Additionally, it is helpful to refrain from walking barefoot indoors or outdoors. It is strongly suggested that all diabetic patients be under the care of a podiatrist who can help them properly manage this condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Plantar warts appear on the bottom of the foot. They grow inward as a result of the constant pressure that is exerted on the feet from standing and walking. They are caused by HPV, human papillomavirus, and can enter the body through small cuts in the feet. It is suggested to wear appropriate shoes while in public swimming areas and locker rooms, as this may prevent the spread of the virus. A plantar wart looks like a small area of hardened skin, and it generally has tiny black dots in the center. These are small, clotted blood vessels that are referred to as wart seeds. This type of wart generally causes severe pain and discomfort, and it may be difficult to walk. Patients who have a compromised immune system, in addition to people who are diabetic, may be prone to getting plantar warts. It is suggested that if you have a plantar wart to speak with a podiatrist who can guide you toward the best treatment methods.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
Treatment
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
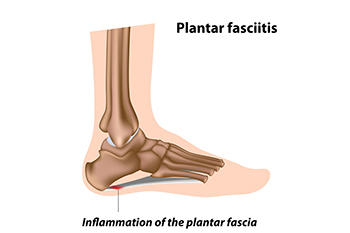
Plantar fasciitis is inflammation of the plantar fascia, the band of fibrous tissue that runs the length of the bottom of the foot to the heel bone. This condition typically develops from over-stretching of that area, and can result in heel and arch pain and heel spurs. Excessive stretching of the plantar fascia can happen for numerous reasons, including flat feet, a sudden increase in physical activity, high body weight and its pressure on the foot, and footwear that is ill fitting. Pain with plantar fasciitis is often its worst first thing after arising from sleep and can diminish a bit as the day wears on. Treatments might be orthotics to reduce over-pronation, cushioning the heel to absorb shock, wearing supportive shoes that accommodate the foot well, losing weight, stretching exercises, and night splints. Since it is vital to determine the cause of plantar fasciitis to treat it properly, it is suggested that a podiatrist be consulted for evaluation.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.

If one’s diabetes is not carefully managed through diet, exercise, and insulin treatment, an all-too-common complication can be a foot ulcer. Ulcers develop because skin tissue breaks down and layers of skin underneath are exposed due to poor circulation, high blood sugar, nerve damage, and irritated or hurt feet. Foot ulcers usually develop under big toes or the balls of the feet. Symptoms to watch for are unusual swelling, irritation, redness, discoloration, drainage from the foot, and odors emanating from the feet. The most visible sign of a foot ulcer is when black tissue (known as “eschar”) surrounds the ulcer because of poor blood flow to the area. However, signs of a foot ulcer are not always present or obvious. Good foot care, including wearing properly fitting, quality shoes, maintaining good foot hygiene, proper trimming of toenails, as well as attention paid to other aspects of physical health, such as heart and kidney disease and obesity, can help with the prevention of foot ulcers. Treatment depends on the cause and severity of the ulcer. It is highly suggested to consult with a podiatrist for proper diagnosis and to obtain a treatment plan.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.