Middlefield (860) 349-8500
Wallingford (203) 294-4977
Middlefield (860) 349-8500
Wallingford (203) 294-4977

Older adults are at an increased risk of developing foot problems. If you have heel pain or pain that is located at the back of your feet, chances are that it may be one of three conditions: plantar fasciitis, bursitis, or an Achilles tendon injury. Plantar fasciitis is the most common form of heel pain. This occurs when the plantar fascia tissue on the bottom of the foot gets injured or irritated and inflamed, typically through overuse. Plantar fasciitis pain is usually more intense in the morning or after periods of rest. Your podiatrist may treat it with custom orthotics, physical therapy, corticosteroid injections, shockwave therapy, or by other means. Bursitis is an inflammatory condition that affects the bursa sac between your Achilles tendon and heel bone at the back of your foot. This is a fluid filled sac that cushions joints and bones, helps protect the tendon, and reduces friction. This bursa can become inflamed, painful, swollen, or red from repetitive motions or direct pressure. The Achilles tendon can suffer from various injuries such as ruptures, tendonitis, or enthesopathy, which are typically caused by intense or repetitive strain on the tendon. If you feel any of the symptoms described here, have a podiatrist examine you and perform whatever tests are necessary to properly diagnose your condition and devise an effective treatment plan.
Many people suffer from bouts of heel pain. For more information, contact Dr. Gordon Fosdick of Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.

Bunions are a foot deformity caused by a misalignment of bones that connect at the joint of the base of the big toe. This deformity causes a bony protrusion at this joint, which then causes the big toe to lean toward the other toes, rather than pointing straight forward. Certain factors can make a person more likely to develop a bunion, such as wearing high-heeled shoes regularly, overpronating, and having certain genetic factors, loose ligaments, or other anomalies in foot structure. Aside from having an irregular appearance, a bunion can cause pain, swelling, numbness, or burning in the big toe joint and/or in the first metatarsal bone (in the forefoot). It may also be difficult to walk or find shoes that fit. It is a good idea to begin treating a bunion as soon as possible for the best results in correcting it. If you already have a fully developed bunion, or believe one is forming, make an appointment with your podiatrist for an examination and evaluation.
If you are suffering from bunions, contact Dr. Gordon Fosdick of Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.

Most sprained ankles occur when the ankle rolls outward as the foot twists inward. This causes the ligaments on the outside of the ankle to stretch and possibly tear. With a mild sprain, the ankle may be sore and stiff. It may swell slightly, but you should be able to walk with minor pain. As the severity of the sprain increases, your ankle may become bruised and tender, making walking far more painful. With a severe sprain, the ankle joint will feel unstable, and bearing weight is not possible. Ankle sprains can take a while to heal, but this long process is important to avoid re-spraining the ankle or developing chronic ankle problems. If you hear a popping sound at the time of the sprain, please see a podiatrist immediately. You will undergo an exam and be given a treatment schedule that may include pain medication, exercises, or bracing to protect the joint and allow it to heal properly. In some cases surgery may be required.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
Preventing a Sprain
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
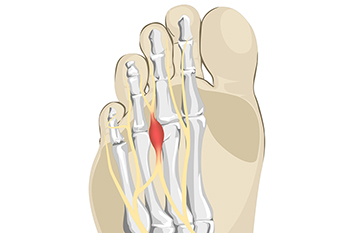
The foot condition that is known as Morton’s neuroma affects the nerve between the third and fourth toes. In severe cases, it is quite painful. This can possibly be treated without surgery in the beginning stages. It happens as a result of wearing shoes that do not have adequate room for the toes to move freely in. High heels fit into this category, and it is suggested to refrain from frequently wearing them. The nerve can gradually become compressed, and it will feel like there is a pebble in the sock or shoe. Additional symptoms can consist of burning pain and numbness in the toes. The pain may radiate to the ball of the foot, and it can be difficult to complete daily activities. A qualified doctor can perform a diagnosis by having an X-ray taken, and this can be helpful in ruling out a stress fracture. An MRI or ultrasound can also be performed, and these can eliminate conditions that may include bursitis and Freiberg’s disease. Some patients find it helpful to stretch the Achilles tendon and plantar fascia, which are located on the bottom of the foot. This may help to reduce a portion of the pain. If you have Morton’s neuroma, it is suggested that you meet with a podiatrist who can recommend the best treatment for you.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Gordon Fosdick of Affiliated Foot Care Center. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.

The feet are considered to be the foundation of the body. Their function is to provide stability and balance to the body, in addition to making it possible to stand, walk and run. Children’s feet grow rapidly to keep up with the rest of their bodies, and will grow faster during puberty. As the child approaches adulthood, the bones in the feet become larger, and will continue to grow until the age of approximately twenty. There are 26 bones in each foot, and the bones in both feet add up to one quarter of the bones in the body. An interesting fact is the feet have the most sweat glands per square centimeter, and 125,000 of them are located on each sole. Additionally, the feet have 8000 nerve endings, and this can contribute to the feet being one of the most ticklish areas of the body. Research has indicated that toenails grow slower than fingernails, and a toenail can take 12 to 18 months to fully grow. If you would like to know more about foot structure, and interesting information about the feet, please consult with a podiatrist.
If you have any concerns about your feet, contact Dr. Gordon Fosdick from Affiliated Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Middlefield and Wallingford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.